Posted on 4/23 by Bridget Landry of the Business Innovation Factory
RWJF Narrative Playbook from Business Innovation Factory on Vimeo.
In healthcare, numbers matter. They are the measures of physical condition – blood pressure, temperature, height and weight – in a patient profile. They govern the amount of time a provider spends with each patient daily (for medical residents, an average of eight minutes) in order to elicit the information needed for assessments and diagnoses.
Increasingly, research shows that a vital aspect of that information is the patient context: the environments, values, relationships and experiences that shape who patients are and how they live. This context directly impacts health, and shapes the challenges patients face in striving to be well; communicating about life outside the four walls of healthcare is thus integral to healthcare that addresses patients’ individual needs.
Doing so without established frameworks, however, can be challenging – especially when quantitative measurements are also crucial and time is short. In confronting this potential challenge, healthcare narrative methods (also referred to as storytelling) are proven, useful tools. They provide the frameworks to create better feedback loops among patients, providers and their caregivers and to ensure that patients’ needs are continuously identified and addressed.
What Is Healthcare Narrative?
Narratives are the systems of stories that compose our human histories and identities; healthcare narrative methods are the carefully designed prompts and processes that elicit these stories, in ways that positively impacts health, care, and healing.
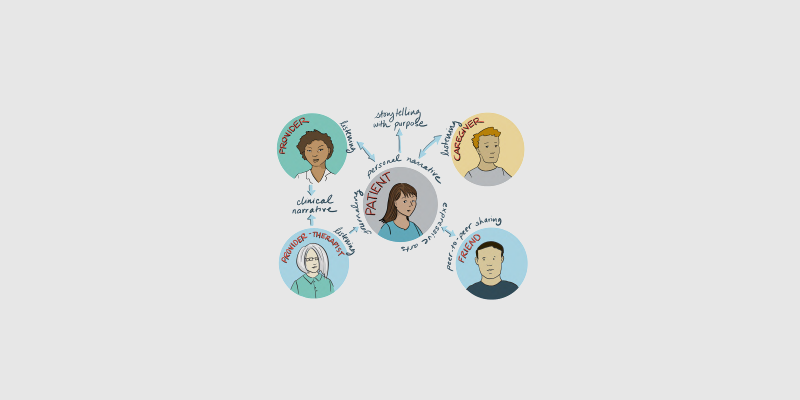
Narrative methods are by nature versatile. Patients, providers, or caregivers can use them. They facilitate processing thoughts and emotions related to healthcare experiences, identifying patterns affecting health or healthcare choices, or reflecting on clinical interactions (and course-correcting when necessary). They include the acts of articulating, reflecting on, listen to, and sharing the stories of our experiences.
With support from the Robert Wood Johnson Foundation, the Patient Experience Lab at the Business Innovation Factory united thirty thought leaders in healthcare narrative methods for a Healthcare Narrative Participatory Design Studio (PDS). In this facilitated space, participants identified and shared healthcare narrative best practices. Several areas of opportunity for healthcare narrative use emerged:
- Ensuring that lines of communication are functioning optimally and continually, so that a patient’s context is understood and adequately addressed by his or her provider in plans for care.
- Enabling communication that allows patients to advocate for their needs, and to allow all parties to process their healthcare experiences in a way that contributes to their well-being.
Below are only two examples of the many healthcare narrative methods that address these areas of opportunity.
Others, including peer-to-peer sharing, expressive arts (e.g. theater and role-playing, visual arts), and active listening, are detailed in the Healthcare Narrative Playbook. Created to codify the insights from the Participatory Design Studio, the Playbook is a practical resource that provides context-specific strategies for healthcare narrative method use.

illustration by Rachel Brian
Examples of Narrative Methods, Use and Impact
- Personal Narrative: the act of telling one’s own stories, both to understand contexts and to reveal needs for care and healing. Stories can be elicited through key questions that invite patients, providers and caregivers to reflect on their lives outside of clinical settings.
Some sample questions to elucidate the stories and contexts that influence the care we give and receive:
- Who are the most important people in your life right now?
- Have there been any significant changes in your life recently? In your relationships? Lifestyle? Finances? Neighborhood?
- What are five things you couldn’t live without?
- What do you hope to be remembered for?
Answering these questions – in writing or conversation, or through other mediums that facilitate expression – and sharing the responses informs the feedback loop between patient and provider with the context that results in effective care plans.
For example: prior to an appointment, a patient might reflect on the story of his life over the past six months, answering the question, “Have there been significant changes in your life recently?” in writing. He realizes that he has moved twice, endured the loss of a parent, and changed jobs; he feels stressed, exhausted, and disoriented.
Because the patient realizes this before his appointment, he brings it up with his provider. The provider subsequently creates a plan of care that includes resources for emotional support; the patient resolves to seek counseling and feels his needs were acknowledged.
This is only one example of the potential use of the personal narrative method – which also isn’t limited to patients. Providers and caregivers can also use questions like those above to elicit their priorities for care. A provider might reflect on the reasons he was drawn to healthcare in the first place and build rapport with patients by sharing how they affect his perspective; a caregiver might realize that her other priorities, like kids’ sports schedules, affect when and how she addresses a sick parent’s medical needs.
- Journaling: Recording thoughts, feelings, experiences and behaviors can reveal patterns that affect health, and research has also shown that the act of journaling in itself reduces stress and improves well-being.
Examples of journals with the potential to improve health outcomes by closing the feedback loop between patients and providers include:
- Health Journal: Patients or caregivers record key aspects of health both in and out of clinical settings. Record symptoms, fluctuations in mood, stressful events, medication changes, etc. Review and look for patterns, use for reference during appointments and other clinical interactions. Refer to when advocating for needs.
- Stress Journal: Patients, providers, or caregivers write for a short time about their most upsetting experiences – e.g. failed treatments, surprising diagnoses. Crafting the stories of these experiences provides emotional catharsis and clarity.
Impact of Narrative
If the stories of our lives define and reveal who we are, healthcare narrative is nothing simpler, or more transformative, than the use of those stories as informational resources to improve care and healing. A relevant narrative, when shared purposefully, has the potential to inform, reveal, heal, or inspire in ways that contribute to better health outcomes – adding a human lens that enriches healthcare experience without detracting from the essential data and time frames.
About the Author:
Bridget Landry is the Patient Experience Lab Associate at the Business Innovation Factory; she writes, learns, shares, and connects to support the Patient Experience Lab’s work. The Patient Experience Lab works with our healthcare system and national funders to explore individuals’ experiences of health and wellness, and to use those insights to design transformative new business models that enable healthy lives.
At the Business Innovation Factory we rely on the co-creation of feedback loops with real-world users, in order to design systems that we all want to be a part of. Interested in learning more about us? Learn more about the work of the Patient Experience Lab here, or follow us on Twitter @BIFpxl.